The vulva and vagina are complex, interconnected systems that play a crucial role in reproductive and overall intimate health. This guide aims to provide a clear, scientifically-grounded exploration of vulvar and vaginal wellness.
Vulva vs Vagina: What’s the Difference?
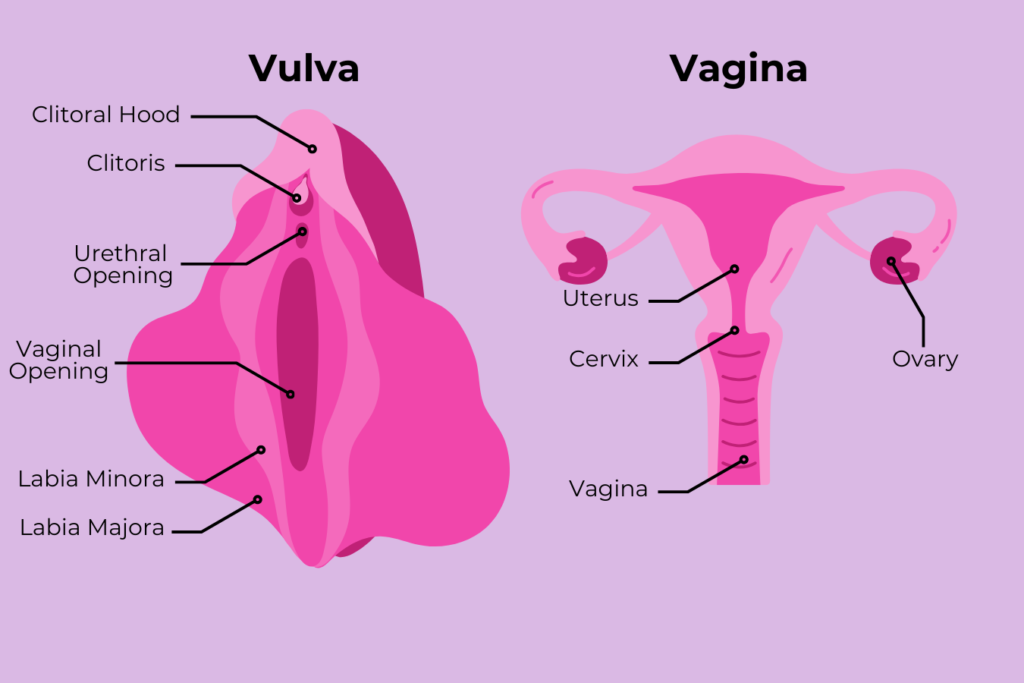
While often used interchangeably, the terms “vulva” and “vagina” refer to distinct parts of the female reproductive anatomy. Let’s clarify these important differences:
Vulva
The vulva encompasses all the external genitalia of the female reproductive system. It includes:
- Labia majora (outer lips)
- Labia minora (inner lips)
- Clitoris
- Urethral opening
- Vaginal opening
- Pubic mound
- Perineum (area between the vaginal opening and anus)
The vulva is the visible part of the female genitalia that you can see from the outside.
Vagina
The vagina, on the other hand, is a specific internal structure. It is:
- A muscular canal that connects the uterus to the outside of the body
- Often referred to as the birth canal
- The passage for menstrual flow and where penetration occurs during sexual intercourse
The vagina is not visible externally and is just one part of the larger vulvar structure.
Why the Distinction Matters
Understanding this difference is crucial for several reasons:
- Anatomical accuracy: Using correct terminology helps in better understanding and communicating about one’s body.
- Health awareness: Knowing the difference aids in identifying and describing health issues more accurately.
- Sexual education: Proper terminology contributes to more comprehensive and effective sexual education.
- Empowerment: Using accurate terms for body parts can lead to greater body confidence and ownership.
By recognizing the distinction between vulva and vagina, we contribute to a more informed and empowered understanding of female anatomy.
The Vaginal Microbiome: A Delicate Ecological Balance
Scientific research has demonstrated the intricate nature of the vaginal ecosystem. According to a landmark study published in Nature Reviews Microbiology, the vaginal microbiome is primarily composed of Lactobacillus species, which maintain a protective acidic environment (pH 3.8-4.5).
Vaginal Discharge: A Physiological Indicator of Health
Vaginal discharge serves critical biological functions:
- Maintaining vaginal cleansing mechanisms
- Regulating moisture levels
- Providing immune protection
Key characteristics of normal discharge include:
- Color: Typically clear or white
- Consistency: Varies from thin to thick
- Odor: Mild or neutral
Hormonal Influences: The Menopausal Transition
Research in the Journal of Menopausal Medicine highlights significant physiological changes during menopause:
- Estrogen decline leads to:
- Increased vaginal pH (>4.5)
- Reduced vaginal epithelial thickness
- Altered microbiome composition
- Potential health implications:
- Increased infection susceptibility
- Vaginal dryness
- Changes in urogenital health
Evidence-Based Recommendations for Vulvar Health
Clinical guidelines suggest the following practices:
- Hygiene Practices
- Gentle external cleansing
- Avoid intrusive cleaning methods
- Use mild, unscented products
- Preventative Care
- Regular gynecological examinations
- Wear breathable, natural fiber underwear
- Practice safe sexual health protocols
Clinical Red Flags Requiring Medical Consultation
Physicians recommend immediate medical evaluation if experiencing:
- Persistent discharge changes
- Unusual odors
- Persistent itching or discomfort
- Pain during urination or intercourse
Common Vulvovaginal Conditions
Scientific classification of typical conditions:
- Bacterial Vaginosis
- Characterized by: Elevated pH (>4.5)
- Indicative signs: Gray discharge, fishy odor
- Vulvovaginal Candidiasis
- pH typically: Around 4.0
- Characteristic discharge: Thick, white
- Associated symptoms: Localized itching
- Trichomoniasis
- pH range: 5.0-6.0
- Discharge: Green/yellow, frothy
- Potential odor: Distinct and unpleasant
Conclusion
Individual variations in vulvar and vaginal health are normal and expected. While this guide provides comprehensive insights, personalized medical consultation remains the most reliable approach for addressing specific health concerns.
Proactive health awareness, regular medical check-ups, and an understanding of bodily changes contribute significantly to overall reproductive wellness.
Sources
- Ravel, J., et al. (2011). “Vaginal microbiome of reproductive-age women.” Proceedings of the National Academy of Sciences, 108(Supplement 1), 4680-4687.
- Santoro, N. (2016). “Perimenopause: From Research to Practice.” Journal of Women’s Health, 25(9), 843-847.
- https://journals.lww.com/jomh/fulltext/2020/11030/vaginal_ph_as_a_diagnostic_tool_for_menopause__a.4.aspx
- https://hsph.harvard.edu/news/vaginal-microbiome-research-uncovers-new-findings-for-womens-health/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10894559/
- https://www.actualgyn.com/en/article/2024/300
- Personal Experience